Antimicrobial resistance (AMR) is the reduced ability of antimicrobials to kill or inhibit the development of microbes consisting of bacteria, viruses, fungi, and parasites. This situation is very dangerous because if it cannot be prevented and controlled, antimicrobial resistance is a threat to the health of all creatures in the world (global health problem). In such condition, the situation is called post-antibiotic era in which most creatures in the world lose their lives due to infectious diseases that cannot be cured by any type of antimicrobial, and it seems happening at that time.
From observations, cases of death associated with antimicrobial resistance each year are in the top 5 cases of diseases that cause death including cancer, diabetes, diarrhea, and traffic accidents (J. O’Neil, 2014. Antimicrobial Resistance: Tackling a crisis for the health and wealth of nations). At the same time, there are not enough new antibiotics being developed to combat bacterial resistance.
Therefore, the antibiotics that are already available should be used more responsibly and managed carefully to extend their life for patients who really need them. Patients should be prescribed antibiotics only when indicated, because they can cause serious side effects.
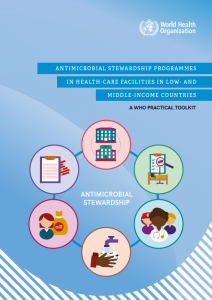
The World Health Organization (WHO) and countries around the world have been struggling to save antimicrobials since five decades ago in the fields of health, agriculture, livestock, fisheries, and the environment. In 2020, the WHO issued antibiotic stewardship guidelines called ANTIMICROBIAL STEWARDSHIP PROGRAMMES. These guidelines were created to implement antimicrobial stewardship (AMS) in health or care facilities intended to help low- and middle-income countries support the implementation of Goal 4 of the Global AMR Action Plan: optimising the use of antimicrobial drugs.
The Ministry of Health of the Republic of Indonesia has started the Antimicrobial Resistance Control Programme in 2005. In 2020, the Ministry of Health of the Republic of Indonesia published the Antimicrobial Stewardship Guidebook. This guideline was published to explain the position, responsibilities, membership, duties and functions, implementation, and monitoring and evaluation of PGA team activities to assist KPRA in optimising the wise use of antimicrobials, which has the effect of reducing selective pressure on microbes, so as to control the development of antimicrobial resistance. The guideline states that every hospital must have a PGA (Antimicrobial Stewardship) team chaired by a specialist in the field of infection with health team members from clinical elements such as clinical pharmacy, clinical microbiology, pathology, or clinical pharmacology.